
Life is full of milestones. One of the least talked about—but most impactful—of these is the transition to menopause. But as important and life-changing as this is, most women have no preparation and little idea of what to expect.
A survey conducted recently by the American Association of Retired Persons (AARP) found that only 18% of women over 35 felt well-informed about the impact of hormonal changes that come with aging. When presented with a list of 28 changes that may result from hormonal decline, 84% of the women recognized at least one, but 16% did not know that any of these conditions were connected to age-related hormone decline and only 7% knew that all were related to hormones.
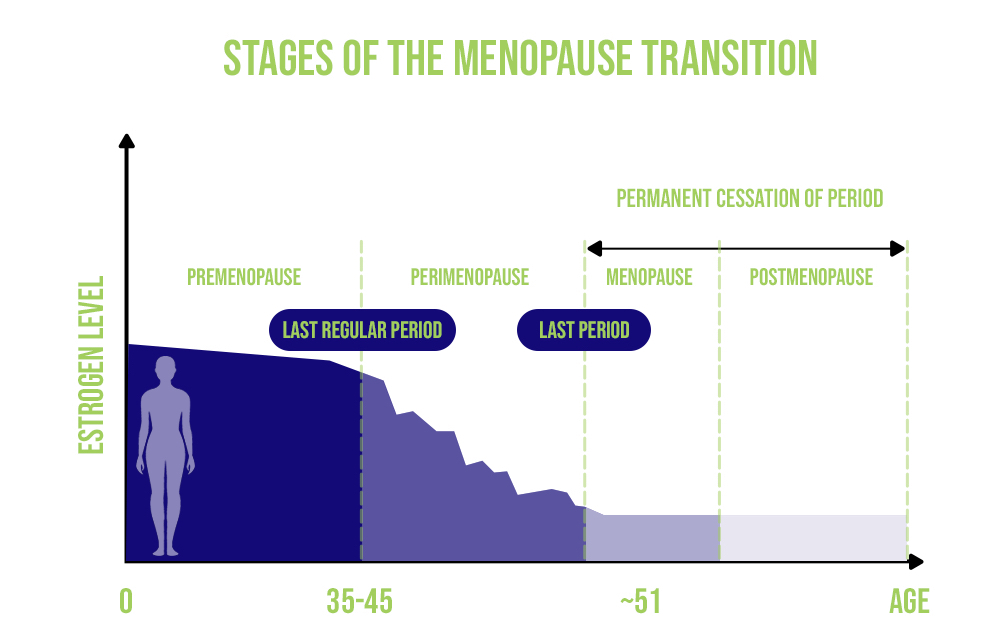
Perhaps the transition is approaching for you. Maybe you have felt early signs that change is coming or are experiencing significant symptoms that are out of the ordinary for you. If you are wondering what comes next or feeling unprepared to deal with this stage of life, you are not alone. Taking a closer look at the menopause hormone levels chart will help you to visualize and better understand what is happening in your body during this transformative time.
Understanding the Menopause Hormone Levels Chart
As women progress through their lives, the sex hormones, especially estrogen, have a major impact, influencing changes that affect many organs and tissues. This is particularly true in the years leading up to menopause.
Premenopause
A woman’s reproductive years occur before menopause. This stage begins at puberty when levels of pituitary hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH), increase, stimulating the production of sex hormones. The resulting increase of sex hormones, (primarily estrogen) causes sexual maturation.
During this stage, there are monthly hormone cycles of estrogen and progesterone, as well as LH and FSH, that trigger ovulation and menstruation. Hormone imbalance is possible at any time in your premenopausal years but is especially likely near the beginning or the end of this stage.
Early Perimenopause
Hormone specialists often say that perimenopause—the years leading up to menopause—begins when declining ovarian function leads to irregular periods. The length and frequency of periods may change, and they may come with heavier bleeding.
Hormones can fluctuate significantly during perimenopause. Estrogen levels fall, triggering the pituitary to produce FSH, which stimulates the follicles to produce more estrogen. This feedback mechanism may create a rollercoaster of hormone fluctuations that lead to uncomfortable physical, emotional, and cognitive symptoms, including hot flashes, mood changes, anxiety, sleep disruptions, vaginal dryness, low sex drive, and memory problems.
Late Perimenopause
Perimenopause lasts on average 3-4 years, but it can span more than a decade for some women. As hormone levels wind down in late menopause, new symptoms can emerge and existing symptoms can change in severity.
Vasomotor symptoms such as hot flashes and night sweats typically peak during this time. Researchers have found that skeletal muscle mass may be particularly vulnerable during late perimenopause. While weight gain is not necessarily associated with changing hormone levels, weight distribution is. Instead of gaining weight in the hips and thighs, as many women do in premenopause, hormonal changes during perimenopause tend to cause an increase in abdominal fat.
Early Postmenopause
Once your periods have stopped for a period of twelve consecutive months, you have officially entered menopause. Hormone fluctuations stop and the body adjusts to the low level of estrogen.
In the early postmenopause period, you may still experience vasomotor symptoms, but other symptoms may start to improve. For example, researchers have found that women in the early postmenopause stage perform more poorly on tests of attention/working memory, verbal learning, verbal memory, and fine motor speed, but these seemed to improve in the late postmenopause stage. Scientists hypothesize that these cognitive changes are primarily due to the effects of declining hormone levels and symptoms that disrupt mood and sleep.
Late Postmenopause
Estrogen, progesterone, and testosterone settle at permanently low levels as women complete the menopause transition, and FSH and LH levels increase. As time goes on, the body adjusts to its new hormonal milieu; some symptoms will resolve, while others, like vaginal tissue changes, will persist or increase. Some studies have found that women report increased body pain, teeth grinding, anxiety, depression, lack of concentration, and sleepiness in late postmenopause than in early postmenopause.
Early/Premature Menopause
While menopause occurs on average at age 51, about 5% of women will experience early menopause (between the ages of 40 and 45) and approximately 1% will undergo premature menopause (before the age of 40). Early and premature menopause are both associated with increased health risks, including cardiovascular disease, neurological disease, psychiatric disease, osteoporosis, and early death.
Women who experience early or premature menopause are often advised to undergo hormone replacement therapy at least until the time that natural menopause would occur. This also applies to women who undergo surgical menopause.
The Power of Information
If you are one of the 82% of women who feel less than fully informed about the menopause transition, you must be your own advocate. As the AARP survey suggests:
- Women want access to “meaningful, relevant, and useful information” about this important change.
- Destigmatizing perimenopause will bring greater knowledge to society as a whole. They note, “With more knowledge and feeling more comfortable talking openly about it, misconceptions can be corrected, resources can be made available, products and services can be developed, and more support for women can be put in place.”
- More open communication regarding aging and hormonal decline will enable women to obtain better care and restore quality of life.
Access to actionable information may mean the difference between “letting nature take its course” and getting the treatment needed to address symptoms and minimize the risk of dangerous health conditions.
 Starting the Dialogue About Menopause
Starting the Dialogue About Menopause
If you suspect that you may be entering perimenopause, now is a good time to schedule a consultation with a hormone specialist. By testing your hormones and discussing your symptoms, medical history, and treatment goals with your doctor, they can create a personalized plan to help you get back on track.
Hormone replacement therapy (HRT) is the gold standard of treatment for many menopause symptoms. According to the critical window theory, otherwise known as the timing hypothesis, starting hormone replacement therapy early in the menopausal transition can help you achieve the best outcomes. But it’s never too late to seek help—HRT can relieve symptoms at any stage.
Talking about menopause can be difficult, but starting the dialogue is the first step toward living the life you want. Finding a caring doctor with expertise in menopause and HRT can ensure you get the guidance you need to understand your options and make this next stage of life as healthy and comfortable as possible.
 Starting the Dialogue About Menopause
Starting the Dialogue About Menopause

